Earlier this week I was meeting a new rheumatologist to possibly replace my doctor who has retired. Ahead of time I picked a few questions to help determine if we might be a good fit. But I was also quietly evaluating the office and its staff – from the logistics of parking, to the receptionist and nurses, and the efficiency of the visit overall.
After negotiating the confusing parking lot and navigating my way through the building to the office, it didn’t take long to get checked in. I was a few minutes early so I read email on my phone and worked a monster Sudoku puzzle. After about 20 minutes, I made eye contact with another patient and we started a brief conversation.
I asked her: How long does it normally take before you’re called back for your appointment? She gave me a sheepish look, so I encouraged her – no, honestly, how long does it take? She said that sometimes it’s “not too long” but that it was an hour for a recent appointment. She asked if I had been waiting long, which I had not, but I noticed that no one had been called back during the 20 minutes I had been waiting and the number of people in the waiting area was growing. (I ended up waiting 30 minutes.)
Not long after this discussion a woman came in and approached the registration desk. She wanted a copy of her lab results and to talk to “whomever it is that usually calls with test results.” The girl at the desk said that person could be any one of them, depending. The previous Friday, the woman had received a phone message regarding lab work and was confused about instructions given to change her medication. She had been trying to call the office all morning and couldn’t get through so she drove up to the office instead.
Based on the conversation, it became apparent that the woman wanted to understand a few basic things: what was abnormal about her lab results, what was the significance of specific tests, why was she being asked to change her meds, what was that supposed to do, and how would she know if the change successfully accomplished what the doctor wanted?
She was obviously concerned and somewhat confused. But rather than offer to let her talk to the nurse, the receptionist responded to her questions with superficial answers that didn’t explain much of anything. I wanted so much to be able to interpret for her what was being said. Her liver enzymes were elevated which is why her doctor wanted her to only take 2 methotrexate tablets that week instead of her usual dose. The patient also wanted to know about SED rate and a few other tests. Her questions had answers, but probably not ones which should have come from a receptionist.
Read this post in its entirety:
Evaluating the Doctor's Office: Who Do You Talk To About Laboratory Results?
Thursday, December 31, 2015
Thursday, December 24, 2015
Much Too Loud!!
Too loud!
Hyperacusis is commonly defined as a heightened, abnormal sensitivity or intolerance to ordinary, everyday sounds that would not bother most people. That means what may sound normal and completely acceptable to you may be perceived as outrageously LOUD and painful to me. People who experience hyperacusis (about 8-15 percent of the general population) often also have tinnitus (ringing in the ears).
Hyperacusis affects people to varying degrees, from mild to severe, and is different than phonophobia (fear of sound) or misophonia (dislike of sound) which usually involve emotional response to specific sounds. People with hearing loss who experience loudness recruitment (an abnormal growth in the perception of loudness) may also experience hyperacusis, but not always.
Although hyperacusis has many known causes and associations, most cases have no known cause. A few diseases and syndromes that are associated with hyperacusis, include migraine, depression, post-traumatic stress disorder, head injury, Lyme disease, Williams syndrome, fibromyalgia, Addison’s disease, autism, myasthenia gravis, and middle cerebral aneurysm. Research suggests that hyperacusis may also be associated with multiple sclerosis.
Not all hyperacusis is the same
Read this post in its entirety:
Do You Think Normal Sounds Are Loud, Painful, or Annoying?
Tuesday, December 22, 2015
Cell-based Therapy and Multiple Sclerosis
Stem cell therapy itself is not entirely new, but use in MS is still experimental and no therapies have been approved in the United States. There are important ongoing clinical trials in the US and a number of patients have traveled abroad to receive treatment. Patients need to be cautious, however, because of the numerous bogus and unscrupulous “stem cell clinics” who heavily recruit patients for their treatments.
What is cell-based therapy?
“Cell-based therapy” refers to the transplantation, delivery or stimulation of various cell types for the purpose of treating MS. It is important to know that there are a variety of cell-based therapies used in MS. To discuss the state of stem-cell research, more than 70 experts convened a meeting - the International Conference on Cell-Based Therapy for Multiple Sclerosis - held in Lisbon and hosted by the National MS Society, ECTRIMS, and Multiple Sclerosis International Federation (MSIF). Progress was reviewed related to the value of specific cell types, including hematopoietic stems cells (derived from the bone marrow), mesenchymal stem cells (derived from many different adult tissues), and oligodendrocyte precursor cells (derived from multiple sources).
Read this post in its entirety:
Stem Cell Research and MS
What is cell-based therapy?
“Cell-based therapy” refers to the transplantation, delivery or stimulation of various cell types for the purpose of treating MS. It is important to know that there are a variety of cell-based therapies used in MS. To discuss the state of stem-cell research, more than 70 experts convened a meeting - the International Conference on Cell-Based Therapy for Multiple Sclerosis - held in Lisbon and hosted by the National MS Society, ECTRIMS, and Multiple Sclerosis International Federation (MSIF). Progress was reviewed related to the value of specific cell types, including hematopoietic stems cells (derived from the bone marrow), mesenchymal stem cells (derived from many different adult tissues), and oligodendrocyte precursor cells (derived from multiple sources).
Read this post in its entirety:
Stem Cell Research and MS
Wednesday, December 16, 2015
Urinary Urgency and MS
For some reason, standing still for a brief period of time makes the situation worse. It seems that if I pause long enough to clinch my legs together, then the next time they relax – for example, in order for me to take a few steps – the muscles holding back the urine relax too and Lisa ends up with soaked underwear and most likely very wet pants.
Losing the ability to control the flow of urine is a common dysfunction in MS. So are problems with storage of urine, emptying of the bladder, or a combination of problems caused by detrusor-external sphincter dyssynergia (DESD) which is a lack of coordination between the different muscle groups that independently control storage and flow.
It is important to talk to your neurologist about any problems you are having with bladder functions. There are treatments which may help to reduce complications. But one thing you should NOT do if you are worried about incontinence is to dramatically limit fluid intake. You need to drink plenty of water to stay appropriately hydrated and to avoid aggravating bowel problems which can often accompany bladder problems.
For me, the onset of bladder problems coincided with a period of time where my MS was progressing somewhat rapidly. I was having several relapses with limited recovery in between. This was years ago, however.
Now, when I begin to have bladder issues, it is often because of a blossoming urinary tract infection or poor attention to my body’s needs on my part. I’ve learned that if the random thought of the bathroom crosses my mind I should act upon it, even if I don’t physically feel the need to go to the restroom…yet. I may not be able to FEEL my need, but my brain is trying to subtly warn me in advance that we’re going to have to make a move soon.
What’s your experience with bladder problems? Are there strategies that you employ to try to manage or prevent problems when you are out and about?
Read this post in its entirety:
Pardon Me, Excuse Me, I've Really Got to GO NOW!
Monday, December 7, 2015
Ways To Connect With The MS Community
3. MS research
One of the first things my neurologist recommended after diagnosis was for me to sign-up for an MS patient registry that conducts longitudinal research through simple surveys. Two of the most prominent patient-based research initiatives in the US are iConquerMS™ which is patient-governed and sponsored by the Accelerated Cure Project (ACP), a non-profit organization in Boston dedicated to research, and the NARCOMS project which is run by the Consortium of MS Centers (CMSC).
4. MS publications
NMSS, MSF, and Multiple Sclerosis Association of America (MSAA) publish quarterly or bi-annual magazines that are delivered to your home. It’s as easy as signing-up. These magazines and select articles can also be viewed online in digital format which is great, especially if you want to share specific information with family and friends and you can link directly to the source. These organizations have also created large libraries of brochures on topics related to practically every aspect of living with MS.
Read this post in its entirety:
5 Wayst to Get Involved in the MS Community
One of the first things my neurologist recommended after diagnosis was for me to sign-up for an MS patient registry that conducts longitudinal research through simple surveys. Two of the most prominent patient-based research initiatives in the US are iConquerMS™ which is patient-governed and sponsored by the Accelerated Cure Project (ACP), a non-profit organization in Boston dedicated to research, and the NARCOMS project which is run by the Consortium of MS Centers (CMSC).
4. MS publications
NMSS, MSF, and Multiple Sclerosis Association of America (MSAA) publish quarterly or bi-annual magazines that are delivered to your home. It’s as easy as signing-up. These magazines and select articles can also be viewed online in digital format which is great, especially if you want to share specific information with family and friends and you can link directly to the source. These organizations have also created large libraries of brochures on topics related to practically every aspect of living with MS.
Read this post in its entirety:
5 Wayst to Get Involved in the MS Community
Stable MRI: Unremarkable and Grossly Normal
Unchanged, grossly normal, unremarkable —– These are some of my favorite words that were included in my most recent MRI report. Very good news. It confirms that my MS has remained stable for another year.
I have been very fortunate. In fact I haven’t had a BIG, steroids-required, symptoms-out-of-control relapse in four years. When I think back to the last one I realize what a difference four years and a minor change in treatment philosophy makes.
Back in 2011, I had a lot of health issues going on and I was suffering from ‘doctor fatigue’ – that feeling you’ve had too many doctor’s appointments and you’re tired of making ‘medical care’ your full-time job and not enough time to take care of yourself.
When I blogged about ‘doctor fatigue’ in 2011, these were some of the things I talked about: 1) failing to schedule an appointment with my rheumatologist in the summer, 2) skipping routine blood monitoring, and 3) not calling the office when I experienced flares. When I finally did schedule an appointment, it was to schedule Rituxan infusions.
At the time, we were waiting to schedule infusions until AFTER I began to experience the return of symptoms (of MS or RA) and I was trying to tough it out. That November, I experienced an MS relapse that affected my walking ability with increased weakness and numbness in my limbs and severe fatigue. A round of solumedrol reduced both my MS and RA symptoms. It was at this point my doctors and I decided that I should try to schedule Rituxan infusions BEFORE symptoms began to return or relapses or flares occurred.
Fast forward to this fall at the end of a very busy string of medical visits and I get good news that reinforces our decision to continue Rituxan infusions every 6 months was the right choice. Rituxan (rituximab) is a B-cell depleting therapy that is used for a variety of conditions including lymphoma and rheumatoid arthritis. Recent trials with a drug that works in the same way, ocrelizumab, showed effectiveness against MS.
Read this post in its entirety:
Happy To Be Unremarkable
Tuesday, December 1, 2015
From Sensory Symptoms to Motor Symptoms: The Most Common Symptoms of MS
Multiple sclerosis is a disease of the central nervous system (CNS) with symptoms that can affect almost anything from head to toes. The disease is so variable that no two people with MS are likely to have exactly the same combination of symptoms. As MS symptoms mimic dozens of other conditions, it is also important to consider that this list is not exclusive to MS.
Here are 50 of the most common MS symptoms:
Sensory problems
Here are 50 of the most common MS symptoms:
Sensory problems
- Abnormal sensations (dysesthesias)
- Numbness, tingling, burning, or tightness
- Pins and needles
- Severe itchiness (pruritus)
- Hypersensitivity to touch
- Pain - acute or chronic, mild to severe
- Loss of proprioception (sense of body position in space)
- Inability to detect vibrations
- Impaired sense of taste or smell
- Trigeminal neuralgia - stabbing pain in the face
- L’Hermitte’s sign - electrical shock-like sensation running down the spine and into the limbs when you bend your neck forward or backward
- The MS hug
Top 50 Symptoms of Multiple Sclerosis
Tuesday, November 24, 2015
Moving Past Guilt to Gratitude
Guilt can be insidious. It serves to keep us down and tends to worsen our impression of its root cause (no matter what that cause, external or internal). I’ll boldly say that much of the time we make ourselves feel guilty even when our loved ones are supportive and wish the best for us.
But what if the guilt is coming not from the several things you can’t do, but from the things you CAN do?
Sounds silly, doesn’t it? Feeling guilty for being ABLE to do things or feeling self-conscious about sharing positive news or about enjoying a bit of that elusive thing called remission.
Not long ago I was at a meeting with other people living with RA during which we were asked as a group about remission. What does remission mean to us? Who had achieved remission?
I have a confession. I was hesitant to say too much because unlike some of the other RA folks in the room, I agreed with my doctor when she determined I was currently in remission. During a recent appointment, I reported no pain or swelling during the past couple of months. (Never mind, I honestly forgot about the minor flare-up I experienced earlier in the summer while we were talking).
I had no tender or swollen joints when she examined me. My inflammatory markers remain low.
I’m doing great!!!
I feel guilty saying so because I know that so many people are not doing well. There is so much pain and angst within our online RA community that sometimes it feels unfair to talk about the good things. But I was encouraged to do just that.
Read this post in its entirety:
From RA Guilt to Gratitude
But what if the guilt is coming not from the several things you can’t do, but from the things you CAN do?
Sounds silly, doesn’t it? Feeling guilty for being ABLE to do things or feeling self-conscious about sharing positive news or about enjoying a bit of that elusive thing called remission.
Not long ago I was at a meeting with other people living with RA during which we were asked as a group about remission. What does remission mean to us? Who had achieved remission?
I have a confession. I was hesitant to say too much because unlike some of the other RA folks in the room, I agreed with my doctor when she determined I was currently in remission. During a recent appointment, I reported no pain or swelling during the past couple of months. (Never mind, I honestly forgot about the minor flare-up I experienced earlier in the summer while we were talking).
I had no tender or swollen joints when she examined me. My inflammatory markers remain low.
I’m doing great!!!
I feel guilty saying so because I know that so many people are not doing well. There is so much pain and angst within our online RA community that sometimes it feels unfair to talk about the good things. But I was encouraged to do just that.
Read this post in its entirety:
From RA Guilt to Gratitude
Friday, November 13, 2015
Being In Limbo Can Be Frightening, No Matter The Diagnosis
I’ve recently been reminded what it feels like to not know exactly what’s going on. To be told, “We found something and want to do more testing. You are scheduled for a procedure next week...that’s a lot like going to the dentist.” To sit in a consultation room shortly after the doctor leaves, pull out your iPhone and google the words she used, and begin to process what you’ve just been told.
Reality check
Last week I went in for my annual mammogram following which I received the standard all-clear in the form of a check-box report. No abnormalities detected. But since my breasts are very dense and I’ve developed lumpy bumpy cysts in recent years, my nurse practitioner had also ordered ABUS (automated breast ultrasound) which is a newer technology that can detect abnormalities in dense breasts that are not seen on mammogram. Ironically, my breasts were too large for the machine to be effective so the traditional hand-held, manual testing was done instead.
Besides the cluster of cysts in the right breast, the ultrasound unexpectedly found two solid masses in my left breast which is what prompted the brief meeting with a radiologist to schedule a core needle breast biopsy in a week. The biopsy took place on Tuesday afternoon and I was told that the report from the pathology lab should be back in 3-4 business days, probably by Friday. Not too long of a wait.
Read this post in its entirety:
Being in Limbo Can Be Frightening
Reality check
Last week I went in for my annual mammogram following which I received the standard all-clear in the form of a check-box report. No abnormalities detected. But since my breasts are very dense and I’ve developed lumpy bumpy cysts in recent years, my nurse practitioner had also ordered ABUS (automated breast ultrasound) which is a newer technology that can detect abnormalities in dense breasts that are not seen on mammogram. Ironically, my breasts were too large for the machine to be effective so the traditional hand-held, manual testing was done instead.
Besides the cluster of cysts in the right breast, the ultrasound unexpectedly found two solid masses in my left breast which is what prompted the brief meeting with a radiologist to schedule a core needle breast biopsy in a week. The biopsy took place on Tuesday afternoon and I was told that the report from the pathology lab should be back in 3-4 business days, probably by Friday. Not too long of a wait.
Read this post in its entirety:
Being in Limbo Can Be Frightening
Wednesday, November 11, 2015
Searching For a New RA Doctor
When my doctor and I have fewer RA-related topics to discuss, she moves onto other topics such as losing weight, exercising more, etc. I took her advice to heart last year and have lost 55 pounds so far by altering the way I eat, riding the exercise bike at home, weighing each day, and keeping detailed records of everything.
Our discussion at this appointment took a different turn. I learned that she is retiring.
RETIRING!! Wait, what, OH NO! She can’t retire. I’ve followed this doctor through three changes in practice. She is great about communicating with my other doctors and with me, having called me after hours on several occasions. She has been my only rheumatologist and she is my golden key to getting the care that I need. She’s awesome.
After I literally blurted out “oh no”, I quickly offered congratulations. It appears that I was supposed to get a letter from the office informing me, but apparently I did not. I am going to need a new rheumatologist, soon. In beginning my search here are some of my initial thoughts and inquiries.
1. Who are the local rheumatologists? My rheumy gave me a list which is very helpful.
2. Who participates in my insurance preferred provider network? Check insurance website.
3. Who has privileges at the local hospital infusion clinic where I’ve been receiving my Rituxan infusions for the past 5+ years? Insurance website provides this information for most doctors.
Then I called the infusion clinic to ask:
4. Who are the doctors in the area who send their RA patients to the clinic for Rituxan infusions? I presume that these doctors are Rituxan-knowledgable, Rituxan-comfortable, and less likely to argue when I ‘tell them’ what my preferred treatment plan continues to be during our initial get-to-know-you appointment.
But in calling the clinic, I learned another consideration:
5. Which doctors in the area continue to have hospital privileges because they chose to go through the extra training required to use the hospital’s updated electronic system?
6. When are the first available appointments for the 3 doctors who match the above criteria?
7. So, who are the doctors who can help me get my Rituxan infusions as close to on-schedule as possible since my doctor is retiring so soon?
I was mildly surprised that nothing about quality, skill, or like-ability had entered my thought process. Nothing about being able to work with my other doctors. Nothing about being familiar with my comorbidities. Nothing about establishing a good patient-doctor relationship.
The main consideration at this time is who can help me to continue to get my treatments in the same way I have for years at a clinic that has excellent facilities and where the nurses know me and are skilled to handle my challenging veins….and who is covered by my insurance policy.
Read this post in its entirety:
Who Can Help Me Get My Next RA Fix?
Our discussion at this appointment took a different turn. I learned that she is retiring.
RETIRING!! Wait, what, OH NO! She can’t retire. I’ve followed this doctor through three changes in practice. She is great about communicating with my other doctors and with me, having called me after hours on several occasions. She has been my only rheumatologist and she is my golden key to getting the care that I need. She’s awesome.
After I literally blurted out “oh no”, I quickly offered congratulations. It appears that I was supposed to get a letter from the office informing me, but apparently I did not. I am going to need a new rheumatologist, soon. In beginning my search here are some of my initial thoughts and inquiries.
1. Who are the local rheumatologists? My rheumy gave me a list which is very helpful.
2. Who participates in my insurance preferred provider network? Check insurance website.
3. Who has privileges at the local hospital infusion clinic where I’ve been receiving my Rituxan infusions for the past 5+ years? Insurance website provides this information for most doctors.
Then I called the infusion clinic to ask:
4. Who are the doctors in the area who send their RA patients to the clinic for Rituxan infusions? I presume that these doctors are Rituxan-knowledgable, Rituxan-comfortable, and less likely to argue when I ‘tell them’ what my preferred treatment plan continues to be during our initial get-to-know-you appointment.
But in calling the clinic, I learned another consideration:
5. Which doctors in the area continue to have hospital privileges because they chose to go through the extra training required to use the hospital’s updated electronic system?
6. When are the first available appointments for the 3 doctors who match the above criteria?
7. So, who are the doctors who can help me get my Rituxan infusions as close to on-schedule as possible since my doctor is retiring so soon?
I was mildly surprised that nothing about quality, skill, or like-ability had entered my thought process. Nothing about being able to work with my other doctors. Nothing about being familiar with my comorbidities. Nothing about establishing a good patient-doctor relationship.
The main consideration at this time is who can help me to continue to get my treatments in the same way I have for years at a clinic that has excellent facilities and where the nurses know me and are skilled to handle my challenging veins….and who is covered by my insurance policy.
Read this post in its entirety:
Who Can Help Me Get My Next RA Fix?
Monday, November 9, 2015
Walking To Get Healthy
I’ve been writing about multiple sclerosis and chronic health topics every week for over 8 years. There is very little chance that I’m in denial regarding the state of my health or disability. Only rarely have I overestimated my ability to do something.
I’m fortunate to be a person living with MS who responds well to treatment and has even experienced an unexpected improvement of physical function after changing disease-modifying therapy 6 years ago.
Last year when my doctor recommended that I strive to walk 10,000 steps every day, I was dubious. But I was also not sure how many steps I might be getting on a routine basis because I wasn’t measuring them. When I got a Fitbit, I was excited to be able to see just how much I was moving (or not) around the house on a normal day.
What I quickly discovered was that during a typical day, I really only walk about 3,000 steps while working at home. On days that I’m more active, I reach 5,000 steps; and if I go out and about, I may reach 7,000 steps. I never get close to the recommended 10,000 steps on a normal day.
Earlier in the summer, Rob and I were in Chicago for a conference. We took a brief walk on Saturday afternoon in the downtown area to get in some exercise after a long day of sitting in meetings. Later in the evening we walked down to the Navy Pier area to watch fireworks over the water.
After returning to the hotel, I checked my Fitbit and noticed that I had reached about 9,100 steps. I was so excited. “Rob, we have to go back out. I might actually be able to get in 10,000 steps if we walk up and down the block one more time. Come on, let’s go!”
Read this post in its entirety:
Getting Healthier 10,000 Steps at a Time
I’m fortunate to be a person living with MS who responds well to treatment and has even experienced an unexpected improvement of physical function after changing disease-modifying therapy 6 years ago.
Last year when my doctor recommended that I strive to walk 10,000 steps every day, I was dubious. But I was also not sure how many steps I might be getting on a routine basis because I wasn’t measuring them. When I got a Fitbit, I was excited to be able to see just how much I was moving (or not) around the house on a normal day.
What I quickly discovered was that during a typical day, I really only walk about 3,000 steps while working at home. On days that I’m more active, I reach 5,000 steps; and if I go out and about, I may reach 7,000 steps. I never get close to the recommended 10,000 steps on a normal day.
Earlier in the summer, Rob and I were in Chicago for a conference. We took a brief walk on Saturday afternoon in the downtown area to get in some exercise after a long day of sitting in meetings. Later in the evening we walked down to the Navy Pier area to watch fireworks over the water.
After returning to the hotel, I checked my Fitbit and noticed that I had reached about 9,100 steps. I was so excited. “Rob, we have to go back out. I might actually be able to get in 10,000 steps if we walk up and down the block one more time. Come on, let’s go!”
Read this post in its entirety:
Getting Healthier 10,000 Steps at a Time
Tuesday, November 3, 2015
New ICD-10 RA Diagnosis Codes
How does ICD-10 affect rheumatology patients and their doctors?
Rheumatoid arthritis (RA) was previously represented by the ICD-9-CM code 714.0. Now RA and its many manifestations are represented by more than 300 individual codes that are grouped under two main categories: Rheumatoid arthritis with rheumatoid factor (ICD-10-CM code M05), and Other rheumatoid arthritis (ICD-10-CM code M06).
The increased number of codes allows for greater detail in documenting the specific manifestations of RA-related disease activity, such as identifying that the left shoulder joint is affected, or that a patient has rheumatoid lung involvement, or whether a patient tested positive for rheumatoid factor.
In my own case of RA, my 714.0 Rheumatoid Arthritis diagnosis has now been changed to “M06.09 Rheumatoid arthritis without rheumatoid factor of multiple sites.”
Examples of other ICD-10-CM codes related to RA disease manifestations:
M05.10 – Rheumatoid lung disease with rheumatoid arthritis of unspecified site
M05.352 – Rheumatoid heart disease with rheumatoid arthritis of left hip
M05.419 – Rheumatoid myopathy with rheumatoid arthritis of unspecified shoulder
M05.719 – Rheumatoid arthritis with rheumatoid factor of unspecified shoulder without organ or systems involvement
M06.071 – Rheumatoid arthritis without rheumatoid factor of right ankle and foot
M06.239 – Rheumatoid bursitis of unspecified wrist
M06.331 – Rheumatoid nodule of right wrist
M71.20 – Synovial cyst of popliteal space [Baker] of unspecified knee
I’m not sure what code would apply if you had seronegative negative RA with rheumatoid lung involvement as the code for rheumatoid lung disease with rheumatoid arthritis is M05.1 which falls under the classification of M05 which is Rheumatoid arthritis with rheumatoid factor.
With all of this in mind, no wonder my soon-to-be-retired rheumatologist said that if she had known exactly when all of this was coming, she might have retired a month sooner.
What do you think? Would having this greater amount of detail hiding in the numbers lead to improved quality of care?
Read this post in its entirety:
What's Your New RA Code?
Rheumatoid arthritis (RA) was previously represented by the ICD-9-CM code 714.0. Now RA and its many manifestations are represented by more than 300 individual codes that are grouped under two main categories: Rheumatoid arthritis with rheumatoid factor (ICD-10-CM code M05), and Other rheumatoid arthritis (ICD-10-CM code M06).
The increased number of codes allows for greater detail in documenting the specific manifestations of RA-related disease activity, such as identifying that the left shoulder joint is affected, or that a patient has rheumatoid lung involvement, or whether a patient tested positive for rheumatoid factor.
In my own case of RA, my 714.0 Rheumatoid Arthritis diagnosis has now been changed to “M06.09 Rheumatoid arthritis without rheumatoid factor of multiple sites.”
Examples of other ICD-10-CM codes related to RA disease manifestations:
M05.10 – Rheumatoid lung disease with rheumatoid arthritis of unspecified site
M05.352 – Rheumatoid heart disease with rheumatoid arthritis of left hip
M05.419 – Rheumatoid myopathy with rheumatoid arthritis of unspecified shoulder
M05.719 – Rheumatoid arthritis with rheumatoid factor of unspecified shoulder without organ or systems involvement
M06.071 – Rheumatoid arthritis without rheumatoid factor of right ankle and foot
M06.239 – Rheumatoid bursitis of unspecified wrist
M06.331 – Rheumatoid nodule of right wrist
M71.20 – Synovial cyst of popliteal space [Baker] of unspecified knee
I’m not sure what code would apply if you had seronegative negative RA with rheumatoid lung involvement as the code for rheumatoid lung disease with rheumatoid arthritis is M05.1 which falls under the classification of M05 which is Rheumatoid arthritis with rheumatoid factor.
With all of this in mind, no wonder my soon-to-be-retired rheumatologist said that if she had known exactly when all of this was coming, she might have retired a month sooner.
What do you think? Would having this greater amount of detail hiding in the numbers lead to improved quality of care?
Read this post in its entirety:
What's Your New RA Code?
Monday, November 2, 2015
Avoiding Catching Colds in Public
I’m a homebody...
It’s no big secret that I don’t get “out” much. I’m a work-at-home writer and musician who has practically everything she needs within a few dozen steps. I’m not sure that I’m truly missing out on too much because I frequently find public spaces to be overstimulating (except that I love that overstimulation when I’m in the middle of it playing my horn). The most common places I frequent on a regular basis, however, include the grocery store, doctors’ offices, and local restaurants.
I usually dread doing things like going shopping at the mall or being in large crowds. Overstimulation aside, there’s another reason that I avoid spending too much time in busy public places. People are often sick and the world is covered in germs. Ok, so that’s two reasons.
Don’t get me wrong; I’m not a germaphobe. I just notice a very predictable pattern to going out into the world. About two days after I’ve been on a public outing, I notice that my lymph nodes become slightly swollen and my sinuses may start dripping down the back of my throat. The effect is not terrible, but it does have me reaching for extra vitamins and OTC medication.
Dealing with a reduced immune system
A number of the medications I take work to reduce the immune system and a potential side-effect is frequent infections. Because of this, and the fact that I teach several children (frequently carriers of all the viruses that spread through the schools), I’ve worked with my students’ parents to encourage them to cancel lessons if the child has been sick, has had a fever within 24 hours, stayed home from school, or otherwise isn’t feeling well enough to be able to concentrate during the lesson.
Also, it is standard procedure that all piano students wash their hands with soap and water BEFORE touching my piano keyboard to try to further reduce the spread of germs. Some students and parents have taken this more seriously than others and I’ve had to crack down on kids who simply disregarded my instructions. I’ve also taught the children to never cough or sneeze on the teacher or the piano keyboard. Ever.
Read this post in its entirety:
Picking Up Colds in Public Places
It’s no big secret that I don’t get “out” much. I’m a work-at-home writer and musician who has practically everything she needs within a few dozen steps. I’m not sure that I’m truly missing out on too much because I frequently find public spaces to be overstimulating (except that I love that overstimulation when I’m in the middle of it playing my horn). The most common places I frequent on a regular basis, however, include the grocery store, doctors’ offices, and local restaurants.
I usually dread doing things like going shopping at the mall or being in large crowds. Overstimulation aside, there’s another reason that I avoid spending too much time in busy public places. People are often sick and the world is covered in germs. Ok, so that’s two reasons.
Don’t get me wrong; I’m not a germaphobe. I just notice a very predictable pattern to going out into the world. About two days after I’ve been on a public outing, I notice that my lymph nodes become slightly swollen and my sinuses may start dripping down the back of my throat. The effect is not terrible, but it does have me reaching for extra vitamins and OTC medication.
Dealing with a reduced immune system
A number of the medications I take work to reduce the immune system and a potential side-effect is frequent infections. Because of this, and the fact that I teach several children (frequently carriers of all the viruses that spread through the schools), I’ve worked with my students’ parents to encourage them to cancel lessons if the child has been sick, has had a fever within 24 hours, stayed home from school, or otherwise isn’t feeling well enough to be able to concentrate during the lesson.
Also, it is standard procedure that all piano students wash their hands with soap and water BEFORE touching my piano keyboard to try to further reduce the spread of germs. Some students and parents have taken this more seriously than others and I’ve had to crack down on kids who simply disregarded my instructions. I’ve also taught the children to never cough or sneeze on the teacher or the piano keyboard. Ever.
Read this post in its entirety:
Picking Up Colds in Public Places
Friday, October 30, 2015
Invisible MS Symptoms Mask Disabiltiy
MS is such an invisible disease. Very few of the symptoms can be seen or detected by others, and only if they are really paying attention, they may notice tremors, inability to walk, balance impairment, speech problems, or bladder/bowel issues. Many MS symptoms cannot be seen, such as pain, spasticity, numbness, itchiness, fatigue, vision problems, dizziness, cognitive problems, or emotional changes.
Most of the time I do not look disabled. I am blessed to be able to move around easily, only getting noticeably fatigued with severe heat or exertion. Symptoms such as spasticity or pain respond to medication, exercise, and rest. Very rarely have I lost bladder control in public and even then I was able to go home to get cleaned up and change clothes.
To look at me, you can’t tell that sensation is diminished in my feet and ankles. My proprioception is affected and I dare not stand with my feet together and close my eyes for risk of losing my balance and falling. I am careful how I place my feet on the ground to avoid the ‘kissing the sidewalk’ symptom which I’ve experienced on a number of occasions. Those face plants are no fun and can cause extreme embarrassment and pain.
When invisible symptoms are hard for others to see...or hear.
Last weekend one of my invisible symptoms - impaired balance - caused a public disruption. I was in the airport in Newark, New Jersey, when TSA agents at the security checkpoint repeatedly asked me to stand in the body scanner machine. I’m not sure what went wrong the very first time I stood there. But in repeated attempts in the machine, the agents complained that either my feet were not far enough apart, or my hands weren’t high enough, or I wobbled which made the image blurry.
Read this post in its entirety:
Invisible MS Symptoms Can Cause Frustration and Mask Disability
Most of the time I do not look disabled. I am blessed to be able to move around easily, only getting noticeably fatigued with severe heat or exertion. Symptoms such as spasticity or pain respond to medication, exercise, and rest. Very rarely have I lost bladder control in public and even then I was able to go home to get cleaned up and change clothes.
To look at me, you can’t tell that sensation is diminished in my feet and ankles. My proprioception is affected and I dare not stand with my feet together and close my eyes for risk of losing my balance and falling. I am careful how I place my feet on the ground to avoid the ‘kissing the sidewalk’ symptom which I’ve experienced on a number of occasions. Those face plants are no fun and can cause extreme embarrassment and pain.
When invisible symptoms are hard for others to see...or hear.
Last weekend one of my invisible symptoms - impaired balance - caused a public disruption. I was in the airport in Newark, New Jersey, when TSA agents at the security checkpoint repeatedly asked me to stand in the body scanner machine. I’m not sure what went wrong the very first time I stood there. But in repeated attempts in the machine, the agents complained that either my feet were not far enough apart, or my hands weren’t high enough, or I wobbled which made the image blurry.
Read this post in its entirety:
Invisible MS Symptoms Can Cause Frustration and Mask Disability
Thursday, October 22, 2015
MS Patient Develops Guided Imagery Program
Treatments for MS that fall outside of conventional medicine are often considered complementary or alternative therapies. Guided imagery is an integrative mind-body therapy that has demonstrated the ability to reduce pain, stress, anxiety, and depression in patients dealing with a variety of disorders. While patients look to integrative medicine to help improve their lives, it is important that research is conducted to demonstrate the benefit of specific interventions, especially those used within the MS communities.
Paula Marie Jackson, diagnosed with MS in 1999, is a certified hypnotherapist who has developed a novel guided imagery protocol for MS patients she calls Healing Light Guided Imagery (HLGI). Ms. Jackson collaborated with researchers from the MS Center at University of California San Diego (UCSD) and the Center of Excellence for Research in Training in Integrative Health to conduct a small self-funded pilot study comparing the effects of HLGI and those of journaling on quality of life, fatigue, and depressed mood in 11 MS patients.
What is Healing Light Guided Imagery (HLGI) and how does it differ from other forms of guided imagery, meditation, or hypnosis?
PMJ: Healing Light Guided Imagery (HLGI) is a hybrid therapy combining meditation, mindfulness, and light hypnosis that I began to develop during my own MS diagnosis. As I trained, practiced, and worked to improve this hybrid technique, I found an optimal framework that worked wonders with most of my symptoms and was effective in helping others living with MS. The researchers at UCSD have been referring to it as an Integrated Mindfulness technique that is a simpler version of mindfulness which is easier to learn in a relatively shorter period of time.
Read this post in its entirety:
MS Patient Designs Novel Guided Imagery Program
Monday, October 19, 2015
Guided Imagery Reduces Depression and Fatigue in MS
Complementary and Alternative Medicine (CAM) therapies include a wide variety of interventions — from diets and supplements to meditation and tai chi — aimed at improving health and well-being. CAM therapies may be used alongside (to complement) or instead of (as alternative to) conventional therapies. Many patients with multiple sclerosis may incorporate CAM therapies into their self-care without realizing it. If you meditate, do yoga, or take certain vitamins or supplements to reduce MS symptoms or improve quality of life, you are using CAM.
In 2014, the American Academy of Neurology (AAN) released guidelines for the use of CAM in MS, classifying therapies into three groups: mind-body medicine, biologically-based practices, or manipulative and body-based practices. The National Center for Complementary and Alternative Medicine (NCCAM) defines mind-body therapies as those that integrate the brain, mind, body, and behavior, with the intent to use the mind to affect physical functioning and promote health; examples include meditation, yoga, tai chi, relaxation techniques, biofeedback, and hypnosis.
Guided Imagery (GI) is a traditional mind-body technique that is considered a form of hypnosis. The term ‘guided imagery’ can be found scattered throughout the literature examining the use of CAM therapies in MS. However, a systematic review of mind-body medicine used in MS identified only a single study (Maguire, 1996) that examined the use of GI in MS producing mixed or inconclusive results.
A recent small pilot study conducted at the University of California San Diego (UCSD) examined the effect of a novel guided imagery modality developed by a person living with MS as compared to guided journaling. This study measured the quality of life, fatigue, and depressed mood in 11 patients with MS over the course of 10 weeks. Participants were randomized to weekly 1-hour guided imagery sessions (n=6) or an at-home journaling program focusing on topics of gratitude or positive self-image (n=5).
Read this post in its entirety:
Guided Imagery May Reduce Depression and Fatigue in MS
In 2014, the American Academy of Neurology (AAN) released guidelines for the use of CAM in MS, classifying therapies into three groups: mind-body medicine, biologically-based practices, or manipulative and body-based practices. The National Center for Complementary and Alternative Medicine (NCCAM) defines mind-body therapies as those that integrate the brain, mind, body, and behavior, with the intent to use the mind to affect physical functioning and promote health; examples include meditation, yoga, tai chi, relaxation techniques, biofeedback, and hypnosis.
Guided Imagery (GI) is a traditional mind-body technique that is considered a form of hypnosis. The term ‘guided imagery’ can be found scattered throughout the literature examining the use of CAM therapies in MS. However, a systematic review of mind-body medicine used in MS identified only a single study (Maguire, 1996) that examined the use of GI in MS producing mixed or inconclusive results.
A recent small pilot study conducted at the University of California San Diego (UCSD) examined the effect of a novel guided imagery modality developed by a person living with MS as compared to guided journaling. This study measured the quality of life, fatigue, and depressed mood in 11 patients with MS over the course of 10 weeks. Participants were randomized to weekly 1-hour guided imagery sessions (n=6) or an at-home journaling program focusing on topics of gratitude or positive self-image (n=5).
Read this post in its entirety:
Guided Imagery May Reduce Depression and Fatigue in MS
Tuesday, October 13, 2015
Positive Trial Results for Ocrelizumab in Primary Progressive MS
After lots of hype and buildup ahead of the conference, the pharmaceutical company Roche-Genentech finally revealed a bit more than simply “positive results” from three pivotal Phase III studies of the experimental MS therapy ocrelizumab in relapsing MS and primary progressive MS (PPMS). While relapsing MS has 13 approved therapies and other treatments which are used off-label, such as rituximab, effective treatment for PPMS has continued to be elusive.
What is ocrelizumab?
Ocrelizumab is a humanized (10 percent mouse, 90 percent human-derived) monoclonal antibody designed to target a selective group of immune cells - CD20+ B-cells - which have been implicated in the damage of myelin, the fatty substance that protects nerve cells and helps to speed the transmission of nerve signals throughout the body. In clinical trials, ocrelizumab 600 mg was administered by intravenous (IV) infusion every six months, given as two 300 mg infusions spaced two weeks apart in the ORATORIO trial, while repeat rounds in the OPERA I and II trials were given as a single 600 mg dose infusion.
Ocrelizumab works in the same way as rituximab (Rituxan), a chimeric (100 percent mouse-derived) monoclonal antibody that attaches to CD20 cell surface proteins and causes certain B-cells (but not stem cells or plasma cells) to self-destruct. Rituxan is used to treat rheumatoid arthritis (RA), non-Hodgkin’s lymphoma (NHL), chronic lymphocytic leukemia (CLL), granulomatosis with polyangitis (GPA) and microscopic polyangitis (MPA). Rituxan is also used off-label for a number of other autoimmune diseases including MS and neuromyelitis optica (NMO). Patents protecting Rituxan (jointly marketed by Genentech and Biogen) from generic competition begin to expire in 2015.
Read this post in its entirety:
Is Ocrelizumab The Next Game-Changer in MS Treatments?
What is ocrelizumab?
Ocrelizumab is a humanized (10 percent mouse, 90 percent human-derived) monoclonal antibody designed to target a selective group of immune cells - CD20+ B-cells - which have been implicated in the damage of myelin, the fatty substance that protects nerve cells and helps to speed the transmission of nerve signals throughout the body. In clinical trials, ocrelizumab 600 mg was administered by intravenous (IV) infusion every six months, given as two 300 mg infusions spaced two weeks apart in the ORATORIO trial, while repeat rounds in the OPERA I and II trials were given as a single 600 mg dose infusion.
Ocrelizumab works in the same way as rituximab (Rituxan), a chimeric (100 percent mouse-derived) monoclonal antibody that attaches to CD20 cell surface proteins and causes certain B-cells (but not stem cells or plasma cells) to self-destruct. Rituxan is used to treat rheumatoid arthritis (RA), non-Hodgkin’s lymphoma (NHL), chronic lymphocytic leukemia (CLL), granulomatosis with polyangitis (GPA) and microscopic polyangitis (MPA). Rituxan is also used off-label for a number of other autoimmune diseases including MS and neuromyelitis optica (NMO). Patents protecting Rituxan (jointly marketed by Genentech and Biogen) from generic competition begin to expire in 2015.
Read this post in its entirety:
Is Ocrelizumab The Next Game-Changer in MS Treatments?
Monday, October 12, 2015
Do You Celebrate Your MS-Anniversary?
So I woke up this morning, trying to remember the date. Then I had this itchy little question in the back of my mind, “What’s supposed to happen today?” After which I remembered…
Today is my MS-iversary!!
It was ten years ago on this date that my neurologist simply informed me that, “Now, we can prescribe one of the disease-modifying drugs.” He didn’t say, “You have MS.” He just told me that my follow-up MRI showed more lesions so I qualified to start treatment. Plain and simple. No big fanfare. I was just ready to get moving on things and to start beating back this beast that was taking away my ability to perform.
That appointment in October was somewhat anticlimactic, however. The month earlier I had attended my neurology clinic’s annual MS seminar at which I was introduced to the specialized MS nurse from the clinic (whom I had yet to meet in the office). She asked me, “Do you have MS?” and my response was, “I don’t know yet.” She replied with a kind hand on the shoulder that I would not have received the mailing for the seminar if it wasn’t very likely I have MS.
MS was not a surprise by the time I received the diagnosis. It was just a turning point that opened up new options for what we could do.
So when I think of the anniversary of my MS diagnosis, I almost laugh. Which event exactly do I want to celebrate? How do I want to put MS into perspective within my life’s journey?
If I look back 10 years to the actual diagnosis date and calculate based on adult years, I’ve lived with MS for just over 34% of my adult life, or not quite 20% of my entire life.
If I look back at the case of blinding optic neuritis, I’ve lived with MS symptoms for 32% of my entire life, or 52% of my adult life.
Or if I go back even further – to the time in graduate school when I was having visual disturbances and the opthalmologist at the university clinic ordered MRIs of my brain/optic nerves – I have lived with a suspected neurological condition for 86% of my adult life.
So how long have I had MS? The official answer would be 10 years.
My apologies to my MS for almost forgetting our anniversary. We’ve been on this road together for so long, and have become so comfortable with each other and our many idiosyncrasies, that I almost forgot.
Read this post in its entirety:
How Dare I Forget My MS-iversary?
Today is my MS-iversary!!
It was ten years ago on this date that my neurologist simply informed me that, “Now, we can prescribe one of the disease-modifying drugs.” He didn’t say, “You have MS.” He just told me that my follow-up MRI showed more lesions so I qualified to start treatment. Plain and simple. No big fanfare. I was just ready to get moving on things and to start beating back this beast that was taking away my ability to perform.
That appointment in October was somewhat anticlimactic, however. The month earlier I had attended my neurology clinic’s annual MS seminar at which I was introduced to the specialized MS nurse from the clinic (whom I had yet to meet in the office). She asked me, “Do you have MS?” and my response was, “I don’t know yet.” She replied with a kind hand on the shoulder that I would not have received the mailing for the seminar if it wasn’t very likely I have MS.
MS was not a surprise by the time I received the diagnosis. It was just a turning point that opened up new options for what we could do.
So when I think of the anniversary of my MS diagnosis, I almost laugh. Which event exactly do I want to celebrate? How do I want to put MS into perspective within my life’s journey?
If I look back 10 years to the actual diagnosis date and calculate based on adult years, I’ve lived with MS for just over 34% of my adult life, or not quite 20% of my entire life.
If I look back at the case of blinding optic neuritis, I’ve lived with MS symptoms for 32% of my entire life, or 52% of my adult life.
Or if I go back even further – to the time in graduate school when I was having visual disturbances and the opthalmologist at the university clinic ordered MRIs of my brain/optic nerves – I have lived with a suspected neurological condition for 86% of my adult life.
So how long have I had MS? The official answer would be 10 years.
My apologies to my MS for almost forgetting our anniversary. We’ve been on this road together for so long, and have become so comfortable with each other and our many idiosyncrasies, that I almost forgot.
Read this post in its entirety:
How Dare I Forget My MS-iversary?
Friday, October 9, 2015
Short Tempers and MS
“Sorry, I’m not really angry with you, but please just stop whatever it is that you’re doing that is driving me CRAZY,” says the MS patient who has lost all his/her patience.
Do you ever feel like that? I do, too often (said with a sheepish downward glance).
I never used to be short on patience for myself or for others, but in recent years, I notice that my fuse has gotten terribly short. I can become ill-tempered at the swift turn of a moment.
Anecdotally, a small number of fellow MS patients have expressed experiencing something similar. At times it seems like anger arises very quickly, or that there are fewer filters through which anger is dispersed.
I was curious to see if there were official connections between MS, short tempers, anger, and extreme mood swings documented in the literature. Various MS societies worldwide offer pages of information related to MS and mood disorders including depression, anxiety, emotional lability, and pseudobulbar affect. But these explanations do not seem to fit what I feel every once in a while.
Part of the time, I feel overwhelmed which contributes to my internal flame. For example, I went shopping recently with my mother for new pants. The saleswoman was very attentive, almost TOO attentive, and wanted to make sure that we had what we needed.
Although I imagine that none of us like to feel like we’ve been abandoned in a dressing room, I now wonder if it’s possible to get too much attention.
Tap, tap, tap…..”how’s the ‘jean no.2’ working out for you?” I hadn’t even taken off jeans no.1 yet and was helping my mother with her own selections. “Do you want me to bring you anything else?” I was also fielding questions from my mother asking what I thought of different options and I was quickly beginning to feel overwhelmed.
Eventually I took a big, deep breath and ask my mom to SLOW it DOWN with the questions. Next thing I know she’s moved into recreating a scene from the old TV show “TAXI” where during the written portion of a driving exam, Jim asks, “what does a yellow light mean?” and his co-worker Bobby whispers, “slow down.” Jim’s response is to ask again, “what….does…a….yellow…light….mean?” in an exchange that repeats itself a few times growing ever more ridiculous.
Aargh, funny enough, but not helpful when I’m trying really hard not to snap at persons who don’t deserve it and are just trying to help me the best way they know how.
Read this post in its entirety:
Just Stop It! Short Fuses and MS
Do you ever feel like that? I do, too often (said with a sheepish downward glance).
I never used to be short on patience for myself or for others, but in recent years, I notice that my fuse has gotten terribly short. I can become ill-tempered at the swift turn of a moment.
Anecdotally, a small number of fellow MS patients have expressed experiencing something similar. At times it seems like anger arises very quickly, or that there are fewer filters through which anger is dispersed.
I was curious to see if there were official connections between MS, short tempers, anger, and extreme mood swings documented in the literature. Various MS societies worldwide offer pages of information related to MS and mood disorders including depression, anxiety, emotional lability, and pseudobulbar affect. But these explanations do not seem to fit what I feel every once in a while.
Part of the time, I feel overwhelmed which contributes to my internal flame. For example, I went shopping recently with my mother for new pants. The saleswoman was very attentive, almost TOO attentive, and wanted to make sure that we had what we needed.
Although I imagine that none of us like to feel like we’ve been abandoned in a dressing room, I now wonder if it’s possible to get too much attention.
Tap, tap, tap…..”how’s the ‘jean no.2’ working out for you?” I hadn’t even taken off jeans no.1 yet and was helping my mother with her own selections. “Do you want me to bring you anything else?” I was also fielding questions from my mother asking what I thought of different options and I was quickly beginning to feel overwhelmed.
Eventually I took a big, deep breath and ask my mom to SLOW it DOWN with the questions. Next thing I know she’s moved into recreating a scene from the old TV show “TAXI” where during the written portion of a driving exam, Jim asks, “what does a yellow light mean?” and his co-worker Bobby whispers, “slow down.” Jim’s response is to ask again, “what….does…a….yellow…light….mean?” in an exchange that repeats itself a few times growing ever more ridiculous.
Aargh, funny enough, but not helpful when I’m trying really hard not to snap at persons who don’t deserve it and are just trying to help me the best way they know how.
Read this post in its entirety:
Just Stop It! Short Fuses and MS
Tuesday, October 6, 2015
Three Things My Doctor Got Right
When I was first diagnosed with MS, there was so much I didn’t know about the disease or about my own body. I thought that I knew, but in looking back I had very little idea.
And to confuse matters, it seemed like I was always one doctor’s visit ahead of my neurologist when it came to recognizing what I needed, such as occupational/physical therapy to rebuild strength in my left hand, a disabled parking placard to avoid becoming a walking hazard, and medication to combat spasticity.
Here was our routine: I would notice a subtle symptom or growing problem and mention it during an office visit. He would examine what could be detected and determine that it was not something to be concerned about. Something would happen between visits related to the original concern and I would dutifully report it. He would then prescribe or recommend whatever service or intervention it was that I originally thought I needed.
At the time, these delays were annoying, but it was a bit entertaining to feel as though I was always one step ahead of my doctor. In retrospect, I feel disappointed that perhaps my neurologist was not as responsive to my concerns as he should have been - a disappointing story which is shared repeatedly among patients in the MS community.
However, there are several things which my doctor got right in his advice and recommendations that I didn't fully appreciate at the time. Here are three of those pieces of wisdom.
Read this post in its entirety:
3 Things My Doctor Got Right
And to confuse matters, it seemed like I was always one doctor’s visit ahead of my neurologist when it came to recognizing what I needed, such as occupational/physical therapy to rebuild strength in my left hand, a disabled parking placard to avoid becoming a walking hazard, and medication to combat spasticity.
Here was our routine: I would notice a subtle symptom or growing problem and mention it during an office visit. He would examine what could be detected and determine that it was not something to be concerned about. Something would happen between visits related to the original concern and I would dutifully report it. He would then prescribe or recommend whatever service or intervention it was that I originally thought I needed.
At the time, these delays were annoying, but it was a bit entertaining to feel as though I was always one step ahead of my doctor. In retrospect, I feel disappointed that perhaps my neurologist was not as responsive to my concerns as he should have been - a disappointing story which is shared repeatedly among patients in the MS community.
However, there are several things which my doctor got right in his advice and recommendations that I didn't fully appreciate at the time. Here are three of those pieces of wisdom.
Read this post in its entirety:
3 Things My Doctor Got Right
Friday, September 25, 2015
Six Non-Medical Issues Caused By Multiple Sclerosis
Factors that affect quality of life are not always easily visible. Here are the top non-medical issues that can impact quality of life (QoL) for those diagnosed with multiple sclerosis and their family members.
An emotional journey from the start.
The MS journal is not just a physical one, it can be an emotional one as well. Before diagnosis, there may be feelings of uncertainty and denial of symptoms. At diagnosis, patients may feel afraid, angry, wonder ‘why me?’, and become isolated. For some, receiving the label of MS can feel a burden and cause great fear in the absence of knowledge about the disease.
Understanding the disease and the disease process.
Patients need to be equipped with knowledge and coping skills to live well with MS, but doctors may be reluctant to share too much information to avoid overwhelming them. A survey study of patients and caregivers identified a desire from both groups for medical professionals to be more forthcoming with information about MS in a manner and format that is easy to understand. Patients and caregivers expressed a need to know what MS is, and what the best solution is for them personally.
Uncertainty renewed, again and again.
During the course of the disease, patients may re-experience many of the same emotions from the times of disease onset and diagnosis due to changing circumstances caused by disease activity or social challenges. Patients who visualize their most feared outcomes may have a pessimistic view of MS which in turn may amplify their symptoms and interfere with QoL.
Read this post in its entirety:
6 Non-Medical Issues that Affect Your Life with MS
An emotional journey from the start.
The MS journal is not just a physical one, it can be an emotional one as well. Before diagnosis, there may be feelings of uncertainty and denial of symptoms. At diagnosis, patients may feel afraid, angry, wonder ‘why me?’, and become isolated. For some, receiving the label of MS can feel a burden and cause great fear in the absence of knowledge about the disease.
Understanding the disease and the disease process.
Patients need to be equipped with knowledge and coping skills to live well with MS, but doctors may be reluctant to share too much information to avoid overwhelming them. A survey study of patients and caregivers identified a desire from both groups for medical professionals to be more forthcoming with information about MS in a manner and format that is easy to understand. Patients and caregivers expressed a need to know what MS is, and what the best solution is for them personally.
Uncertainty renewed, again and again.
During the course of the disease, patients may re-experience many of the same emotions from the times of disease onset and diagnosis due to changing circumstances caused by disease activity or social challenges. Patients who visualize their most feared outcomes may have a pessimistic view of MS which in turn may amplify their symptoms and interfere with QoL.
Read this post in its entirety:
6 Non-Medical Issues that Affect Your Life with MS
Wednesday, September 23, 2015
Five Hidden Symptoms of Multiple Sclerosis
Disability progression has an obvious impact of quality of life and is often an outwardly visible sign of MS. But quality of life (QoL) in MS can be influenced by many invisible symptoms. Here are the top hidden issues that may impact quality of life for those diagnosed with multiple sclerosis.
Fatigue.
Fatigue is extremely common affecting 75 to 95 percent of people with MS. It can be one of the most troublesome symptoms regardless of one’s disease course or level of disability. The Social Security Administration recognizes fatigue as a significant cause of unemployment among people with MS. The first step in combating fatigue is working with your doctor to narrow down the cause.
Depression.
One study found that depression was the main factor affecting quality of life in MS patients, more so than disability status, fatigue, or reduced sleep quality. Depression can be caused by neurological damage associated with MS, but may also be caused by the emotional rollercoaster associated with difficult life challenges and the uncertainty of MS. Symptoms of depression may include sadness, irritability, loss of interest, sleeping too much or too little, weight loss or gain, fatigue, physical restlessness, impaired concentration, and thoughts of suicide or death. If you experience any of these symptoms, please talk to your healthcare provider.
Cognitive decline.
Cognitive issues can develop early on in the course of MS and impaired cognition can lead to a vicious cycle of frustration creating a negative impact on QoL. However, it is not always apparent whether cognitive decline is a result of depression, fatigue, neurological impairment, or a combination of factors. Patients should undergo neuropsychological evaluation so that appropriate treatment may be recommended and QoL may be protected.
Research shows that larger brain volume, cognitive reserve gained through life experience (such as years of education), and lifestyle choices (engaging in cognitive leisure activities such as reading) protect against disease-related cognitive impairment in MS patients.
Sexual (dys)function.
Sexual dysfunction, which affects up to 75 percent of women and 90 percent of men with MS, can be distressing for the patient and have a negative impact on family relationships. In fact, sexual dysfunction has been shown to have a greater detrimental effect on mental health aspects of health-related QoL in MS patients than the severity of physical disability. However, patients may be reluctant to discuss sexual dysfunction and doctors may not ask.
Reduced sleep quality.
Sleep disorders, including obstructive sleep apnea (OSA) and insomnia, are common in MS. Reduced sleep quality can lead to fatigue and depression and CPAP therapy can improve these symptoms in patients with sleep apnea. A recent study showed that sleep disorders can reduce QoL of MS patients, especially in areas related to energy and emotion. In patients with OSA, physical abilities can also be negatively affected. Due to the complex relationship between fatigue, depression, and sleep disorders in MS, it can be difficult to detect the root cause in traditional QoL questionnaires.
Read this post in its entirety:
Five Hidden Symptoms of MS
Fatigue.
Fatigue is extremely common affecting 75 to 95 percent of people with MS. It can be one of the most troublesome symptoms regardless of one’s disease course or level of disability. The Social Security Administration recognizes fatigue as a significant cause of unemployment among people with MS. The first step in combating fatigue is working with your doctor to narrow down the cause.
Depression.
One study found that depression was the main factor affecting quality of life in MS patients, more so than disability status, fatigue, or reduced sleep quality. Depression can be caused by neurological damage associated with MS, but may also be caused by the emotional rollercoaster associated with difficult life challenges and the uncertainty of MS. Symptoms of depression may include sadness, irritability, loss of interest, sleeping too much or too little, weight loss or gain, fatigue, physical restlessness, impaired concentration, and thoughts of suicide or death. If you experience any of these symptoms, please talk to your healthcare provider.
Cognitive decline.
Cognitive issues can develop early on in the course of MS and impaired cognition can lead to a vicious cycle of frustration creating a negative impact on QoL. However, it is not always apparent whether cognitive decline is a result of depression, fatigue, neurological impairment, or a combination of factors. Patients should undergo neuropsychological evaluation so that appropriate treatment may be recommended and QoL may be protected.
Research shows that larger brain volume, cognitive reserve gained through life experience (such as years of education), and lifestyle choices (engaging in cognitive leisure activities such as reading) protect against disease-related cognitive impairment in MS patients.
Sexual (dys)function.
Sexual dysfunction, which affects up to 75 percent of women and 90 percent of men with MS, can be distressing for the patient and have a negative impact on family relationships. In fact, sexual dysfunction has been shown to have a greater detrimental effect on mental health aspects of health-related QoL in MS patients than the severity of physical disability. However, patients may be reluctant to discuss sexual dysfunction and doctors may not ask.
Reduced sleep quality.
Sleep disorders, including obstructive sleep apnea (OSA) and insomnia, are common in MS. Reduced sleep quality can lead to fatigue and depression and CPAP therapy can improve these symptoms in patients with sleep apnea. A recent study showed that sleep disorders can reduce QoL of MS patients, especially in areas related to energy and emotion. In patients with OSA, physical abilities can also be negatively affected. Due to the complex relationship between fatigue, depression, and sleep disorders in MS, it can be difficult to detect the root cause in traditional QoL questionnaires.
Read this post in its entirety:
Five Hidden Symptoms of MS
Monday, September 21, 2015
Quality of Life With MS Affected by Hidden Symptoms
A recent study shows that ‘hidden’ factors have the capacity to influence quality of life (QoL) for MS patients. In clinical trials, traditional measures of quality of life for MS patients center around disease activity and physical disability progression. Measuring things such as relapses and lesions is much easier than measuring non-medical issues related to quality of life; but it reflects only part of the patient’s experience.
Quality of life can be complicated. MS patients may respond well to treatment and be free of significant symptoms, but still have poor QoL due to factors such as depression, inability to work, and relationship issues. They may “look fine” but have a reduced quality of life. Conversely, patients who have accumulated significant physical disability may continue to participate fully in life and view their own QoL in a positive light.
While MS patients need to learn to cope with visible and invisible issues related to MS, discussing these issues with family, friends, or medical professionals may be difficult. Patients and providers both may be reluctant to discuss invisible issues during routine clinical visits. In addition, the problems may be complex and difficult to manage because of the lack of efficient solutions.
Read this post in its entirety:
Quality of Life and MS
Tuesday, September 15, 2015
Spammy Posts on Facebook
In the MS community, there has been an increasing number of low-quality websites that are scraping reputable material, such as that provided by MultipleSclerosis.net. The owners of these low-quality websites often create “fake” FB profiles which are used to join MS groups with the singular purpose of posting links to the scraped content.
How does this hurt the MS community?
This practice is bad for the MS community because these low-quality websites may contain ads for questionable products, have malware or viruses, and keep you from discovering relevant high-quality material on reputable websites. These spammy websites seem to exist primarily to get clicks and earn advertising fees.
I began researching several of these websites after noticing that they were being heavily promoted in certain MS-related FB groups. I have identified 46 suspicious websites whose URLs were registered, primarily in Pakistan and Panama, by fewer than 7 individuals. Some registrants have used more than one country in which to register their collection of domains. One domain owner is independently connected to 18 sites (with 9 additional sites suspected) while a group of 5 individuals seem to be connected to 13 sites between them.
The invasion is ongoing.
I have discovered that 36 of these 46 websites were created within the past three months; 18 in August and 6 in September alone. That’s a huge influx of suspicious websites trying to distract the online MS community with stolen or scraped material. In the short time since I began writing this article, 8 additional websites went up accompanied by 30 new fake FB profiles to promote them. Unfortunately, I believe that the admin(s) for a few newer MS groups that aggressively added members this summer are actually connected to this entire scam.
How can you find out who registered a website, when and where?
Every time a domain is registered, the details of that registration must be published in a publicly accessible database called WHOIS. You can go directly to a WHOIS listing by typing www.whois.com/whois/[insertyoururl.com] into a browser. However, there are ways to hide registrant information, so you may only see that the name is protected or private.
Can you spot a fake Facebook profile?
These same handful of domain owners have created at least 80 fake Facebook profiles used to promote the scraped articles published on their low-quality websites. One domain registrant has created at least 32 fake FB profiles, while another team has created 30, that are used to spam MS groups. Here’s an article on ITWorld that explains ways to spot a fake FB profile.
And, a Wordle created from information – website urls, domain registrants, their locations, and fake FB profiles – gleaned through personal research and observation regarding the WORST OFFENDERS in the MS groups:
Wordle Websites.004How can you easily find out if an article was scraped?
The easiest way to find the original article is to use Google to search for a significant portion of the text. This will often bring you directly to the original, reputable website where you may find more high-quality MS-related information.
How can you determine if a website has trustworthy health information?
The Health On the Net (HON) Foundation is a non-profit, non-governmental organization created in 1995 that “promotes and guides the deployment of useful and reliable online health information, and its appropriate and efficient use.” To receive HONcode certification, websites must go through a thorough review and approval process. Having gone through this process for my own blog that has HONcode certification, I can attest that the process is quite rigorous and detailed. Look for an active HONcode on a website.
What SHOULD you do if you notice questionable posts in your favorite group on Facebook?
You should report the post and/or fake FB profiles to the group’s administrator. You may be asked why you reported the particular post or person in question, in which case you can explain your concern; then provide a link to this article to support why you believe it’s important to keep our groups free from predators.
Pause a moment next time before you click “like” or decide to “share” something on Facebook, even if the post is very tempting with a great headline or pretty image. Please freely share links you find from your favorite, trustworthy websites such as MultipleSclerosis.net to help distribute quality information.
Please be aware that all of the information presented above focuses on what I’ve witnessed within the MS community on Facebook. Low-quality websites are being widely promoted through fake FB profiles in many other disease communities of epidemic proportions that exceed my ability to analyze by hand.
As a community of people who deal with chronic illness, we need to stick up for ourselves and help each other to think critically and push back when possible. If you see this going on in your group, please, report it and do not be prey.
Read this post in its entirety:
Buyer Beware: Influx of Suspicious Websites Using Stolen or Scraped Material
How does this hurt the MS community?
This practice is bad for the MS community because these low-quality websites may contain ads for questionable products, have malware or viruses, and keep you from discovering relevant high-quality material on reputable websites. These spammy websites seem to exist primarily to get clicks and earn advertising fees.
I began researching several of these websites after noticing that they were being heavily promoted in certain MS-related FB groups. I have identified 46 suspicious websites whose URLs were registered, primarily in Pakistan and Panama, by fewer than 7 individuals. Some registrants have used more than one country in which to register their collection of domains. One domain owner is independently connected to 18 sites (with 9 additional sites suspected) while a group of 5 individuals seem to be connected to 13 sites between them.
The invasion is ongoing.
I have discovered that 36 of these 46 websites were created within the past three months; 18 in August and 6 in September alone. That’s a huge influx of suspicious websites trying to distract the online MS community with stolen or scraped material. In the short time since I began writing this article, 8 additional websites went up accompanied by 30 new fake FB profiles to promote them. Unfortunately, I believe that the admin(s) for a few newer MS groups that aggressively added members this summer are actually connected to this entire scam.
How can you find out who registered a website, when and where?
Every time a domain is registered, the details of that registration must be published in a publicly accessible database called WHOIS. You can go directly to a WHOIS listing by typing www.whois.com/whois/[insertyoururl.com] into a browser. However, there are ways to hide registrant information, so you may only see that the name is protected or private.
Can you spot a fake Facebook profile?
These same handful of domain owners have created at least 80 fake Facebook profiles used to promote the scraped articles published on their low-quality websites. One domain registrant has created at least 32 fake FB profiles, while another team has created 30, that are used to spam MS groups. Here’s an article on ITWorld that explains ways to spot a fake FB profile.
And, a Wordle created from information – website urls, domain registrants, their locations, and fake FB profiles – gleaned through personal research and observation regarding the WORST OFFENDERS in the MS groups:
Wordle Websites.004How can you easily find out if an article was scraped?
The easiest way to find the original article is to use Google to search for a significant portion of the text. This will often bring you directly to the original, reputable website where you may find more high-quality MS-related information.
How can you determine if a website has trustworthy health information?
The Health On the Net (HON) Foundation is a non-profit, non-governmental organization created in 1995 that “promotes and guides the deployment of useful and reliable online health information, and its appropriate and efficient use.” To receive HONcode certification, websites must go through a thorough review and approval process. Having gone through this process for my own blog that has HONcode certification, I can attest that the process is quite rigorous and detailed. Look for an active HONcode on a website.
What SHOULD you do if you notice questionable posts in your favorite group on Facebook?
You should report the post and/or fake FB profiles to the group’s administrator. You may be asked why you reported the particular post or person in question, in which case you can explain your concern; then provide a link to this article to support why you believe it’s important to keep our groups free from predators.
Pause a moment next time before you click “like” or decide to “share” something on Facebook, even if the post is very tempting with a great headline or pretty image. Please freely share links you find from your favorite, trustworthy websites such as MultipleSclerosis.net to help distribute quality information.
Please be aware that all of the information presented above focuses on what I’ve witnessed within the MS community on Facebook. Low-quality websites are being widely promoted through fake FB profiles in many other disease communities of epidemic proportions that exceed my ability to analyze by hand.
As a community of people who deal with chronic illness, we need to stick up for ourselves and help each other to think critically and push back when possible. If you see this going on in your group, please, report it and do not be prey.
Read this post in its entirety:
Buyer Beware: Influx of Suspicious Websites Using Stolen or Scraped Material
Friday, September 11, 2015
Alemtuzumab and Infusion Reactions
Lemtrada (alemtuzumab 12 mg) is a humanized monoclonal antibody, targeting CD52+ T and B cells, delivered by IV infusion on five consecutive days (course 1) followed by another three consecutive days one year later (course 2). Lemtrada has been approved in several countries for treatment of relapsing-remitting multiple sclerosis (RRMS) and is generally reserved for people with MS who have failed other treatments.
In clinical trials, infusion-associated reactions (IARs) affected 90.1 percent of patients receiving alemtuzumab. The most common IARs were headache, rash, fever (pyrexia), nausea, and flushing; most were mild to moderate in severity. The two main types of IARs are allergic (hypersensitivity) and nonallergic (cytokine release) reactions.
IARs were more frequent during course 1 than during course 2 of treatment; IARs occurred in 84.7-96.3 percent of patients during course 1 compared with 68.6-81.9 percent of patients during course 2. In each treatment course, the greatest numbers of IARs occurred with the first infusion and decreased with each infusion thereafter.
Management of IARs
Nurses play an important role in the detection and management of IARs. Best practices for management of IARs associated with Lemtrada include patient and caregiver education, prophylactic medication—particularly corticosteroids, antihistamines, and antipyretics—to reduce IAR severity, infusion monitoring, and discharge planning.
Severe IARs can generally be managed by slowing the infusion rate or by temporarily stopping the infusion, allowing time for recovery of symptoms, and then restarting at a slower rate.
Read this post in its entirety:
Prevention of Infusion Reactions with Lemtrada
In clinical trials, infusion-associated reactions (IARs) affected 90.1 percent of patients receiving alemtuzumab. The most common IARs were headache, rash, fever (pyrexia), nausea, and flushing; most were mild to moderate in severity. The two main types of IARs are allergic (hypersensitivity) and nonallergic (cytokine release) reactions.
IARs were more frequent during course 1 than during course 2 of treatment; IARs occurred in 84.7-96.3 percent of patients during course 1 compared with 68.6-81.9 percent of patients during course 2. In each treatment course, the greatest numbers of IARs occurred with the first infusion and decreased with each infusion thereafter.
Management of IARs
Nurses play an important role in the detection and management of IARs. Best practices for management of IARs associated with Lemtrada include patient and caregiver education, prophylactic medication—particularly corticosteroids, antihistamines, and antipyretics—to reduce IAR severity, infusion monitoring, and discharge planning.
Severe IARs can generally be managed by slowing the infusion rate or by temporarily stopping the infusion, allowing time for recovery of symptoms, and then restarting at a slower rate.
Read this post in its entirety:
Prevention of Infusion Reactions with Lemtrada
Wednesday, September 9, 2015
Letting Go of Pre-RA Shoes
Every few months, we receive phone calls from various advocacy organizations who are looking for donations of household goods, such as clothing, books, or small appliances, to sell to raise funds for their organization. Oftentimes I agree to prepare a box or two for donation which provides a good opportunity to go through excess in our house and select items that deserve a new home.
This past week when going through stuff I focused on packing up shoes and clothing. For the clothing, it was not too difficult deciding what items to include because this time around, I chose to let go of items which I had simply grown out of. Well, not really grown out of, but rather lost weight out of. Things that simply didn’t fit anymore even with safety pins.
Choosing shoes to donate was a bit more difficult, or rather more sentimental. There were shoes in my collection that I used to wear as part of my ‘all black concert clothing’ attire. Some of these shoes were the most comfortable when I purchased them: slightly narrow width which kept them snug on my heels, a little extra arch support, low heels, and just the right amount of cushion.
These shoes were cute, and somewhat expensive. I loved them so much that I followed my mother’s advice: “If you find something that works well, and that you love, consider buying backups because they most likely won’t be available when the original pair [of shoes] wears out.”
But over the years, these ‘oh so comfortable shoes’ have become torture devices. Each time I’ve tried to wear them, I end up in such pain and with icky blisters that it’s just impossible to bear.
What has changed? Simply put….RA.
There are stories of women whose feet changed shape after pregnancy, but I’ve never been through that so I don’t have firsthand experience. I’ve heard of women whose feet changed shape simply because of age, but mine had been the same for many years.
We don’t often talk about what RA can do to the feet. Some patients may feel like they are walking on hard rocks due to inflammation in the feet. Some patients develop deformities due to damaged joints in the feet caused by the destructive power of RA.
Read this post in its entirety:
Saying Goodbye to Pre-RA Shoes
This past week when going through stuff I focused on packing up shoes and clothing. For the clothing, it was not too difficult deciding what items to include because this time around, I chose to let go of items which I had simply grown out of. Well, not really grown out of, but rather lost weight out of. Things that simply didn’t fit anymore even with safety pins.
Choosing shoes to donate was a bit more difficult, or rather more sentimental. There were shoes in my collection that I used to wear as part of my ‘all black concert clothing’ attire. Some of these shoes were the most comfortable when I purchased them: slightly narrow width which kept them snug on my heels, a little extra arch support, low heels, and just the right amount of cushion.
These shoes were cute, and somewhat expensive. I loved them so much that I followed my mother’s advice: “If you find something that works well, and that you love, consider buying backups because they most likely won’t be available when the original pair [of shoes] wears out.”
But over the years, these ‘oh so comfortable shoes’ have become torture devices. Each time I’ve tried to wear them, I end up in such pain and with icky blisters that it’s just impossible to bear.
What has changed? Simply put….RA.
There are stories of women whose feet changed shape after pregnancy, but I’ve never been through that so I don’t have firsthand experience. I’ve heard of women whose feet changed shape simply because of age, but mine had been the same for many years.
We don’t often talk about what RA can do to the feet. Some patients may feel like they are walking on hard rocks due to inflammation in the feet. Some patients develop deformities due to damaged joints in the feet caused by the destructive power of RA.
Read this post in its entirety:
Saying Goodbye to Pre-RA Shoes
Tuesday, September 8, 2015
Remembering Events in Life Based on Health Status
In looking back on things that have happened over the years. Some may say that “life happened” as it tends to happen for most anybody as the years go on. In our lives, it’s more accurate to say that “sickness happened.”
It seems clear in retrospect that the relentless onset of MS and RA over the course of 18 months, following five years of fluctuating symptoms (such as temporary blindness, heavy legs, painful feet/ankles, achy hands, etc), changed the course of my life irrevocably. Things began to be neglected.
There’s a virtual wall between how I was able to manage life pre-MS versus post-MS. It wasn’t until my mom and I were talking about things around the house that I realized - and truly and honestly acknowledged - that life has become punctuated by health events.
Read this post in its entirety:
Life Punctuated by Health and Sickness
It seems clear in retrospect that the relentless onset of MS and RA over the course of 18 months, following five years of fluctuating symptoms (such as temporary blindness, heavy legs, painful feet/ankles, achy hands, etc), changed the course of my life irrevocably. Things began to be neglected.
There’s a virtual wall between how I was able to manage life pre-MS versus post-MS. It wasn’t until my mom and I were talking about things around the house that I realized - and truly and honestly acknowledged - that life has become punctuated by health events.
Read this post in its entirety:
Life Punctuated by Health and Sickness
Monday, September 7, 2015
Going Without My Parking Pass
I’ve looked everywhere I can think of:
I know that I had the parking pass in my car earlier this summer. I used it when my mother and I vacationed in May. I remember putting it in my purse when I valeted my car at a conference in June.
Fortunately, I don’t use the parking pass very often anymore. And when my mom is with me, her pass is usually available (when we remember it).
My current parking pass (if I could just find it) doesn’t expire until next October in 2016. That’s a long time from now and as you know with MS, you hardly can plan when you might need a little assistance by parking closer to your destination.
But having the pass in my car, not needing it, and choosing to park farther away from my destination to purposefully get more steps in for the day (as I routinely wear my FitBit One each day to roughly measure physical activity), makes me feel more confident.
My parking placard serves as a reminder that MS is not nearly as invasive as it once was in my life.
I haven’t decided what I’m going to do right now though, other than deciding to enjoy the knowledge that I’m doing well.
Read this post in its entirety:
What Have I Done With My Parking Pass?
- In the car – in the normal storage spot, under the seat, between the seats, in the glovebox, backseat? Nope.
- In my purse – outside pocket, inside pocket? Nope. Check all my purses that have been used this summer. Nope.
- Where we keep the keys. Nope. Coffee table. Nope. Pile of mail. Nope.
- Rob’s car. His mom’s car (because I did go somewhere with her last month). My mom’s car. Nope. Nope. Nope.
I know that I had the parking pass in my car earlier this summer. I used it when my mother and I vacationed in May. I remember putting it in my purse when I valeted my car at a conference in June.
Fortunately, I don’t use the parking pass very often anymore. And when my mom is with me, her pass is usually available (when we remember it).
My current parking pass (if I could just find it) doesn’t expire until next October in 2016. That’s a long time from now and as you know with MS, you hardly can plan when you might need a little assistance by parking closer to your destination.
But having the pass in my car, not needing it, and choosing to park farther away from my destination to purposefully get more steps in for the day (as I routinely wear my FitBit One each day to roughly measure physical activity), makes me feel more confident.
My parking placard serves as a reminder that MS is not nearly as invasive as it once was in my life.
I haven’t decided what I’m going to do right now though, other than deciding to enjoy the knowledge that I’m doing well.
Read this post in its entirety:
What Have I Done With My Parking Pass?
Thursday, September 3, 2015
Exercise Helps Urinary Symptoms in MS
One of the most common physical dysfunctions in multiple sclerosis is urinary incontinence (UI) - the leakage of urine at inappropriate times. It is also common in the general population with an estimated 115 million people worldwide reporting UI in 2013, and more than 12.6 percent of the general population in the United States being diagnosed with UI.
An estimated 50-100 percent of people with MS will experience UI. Both men and women can experience UI, but it is more common in women. UI frequently involves pelvic floor muscles that attach to the bottom of the pelvic bones to form a bowl-like structure that lifts to support internal organs and control sphincter muscles.
Lower urinary tract symptoms (LUTS) include frequency, urgency, stress and urge incontinence as well as voiding or obstructive complications. Stress incontinence occurs when the pelvic floor muscles are too weak to stop urine from leaking when you cough, laugh, or sneeze. Urge incontinence, or overactive bladder (OAB), occurs when urine leakage is closely preceded by a powerful urge to pass urine. It’s often a “I gotta go, gotta go, gotta go NOW," type of situation. Functional incontinence involves leakage when you struggle to get to the bathroom in time.
Read this post in its entirety:
Want to Improve Urinary Incontinence Symptoms? Try Physical Therapy
An estimated 50-100 percent of people with MS will experience UI. Both men and women can experience UI, but it is more common in women. UI frequently involves pelvic floor muscles that attach to the bottom of the pelvic bones to form a bowl-like structure that lifts to support internal organs and control sphincter muscles.
Lower urinary tract symptoms (LUTS) include frequency, urgency, stress and urge incontinence as well as voiding or obstructive complications. Stress incontinence occurs when the pelvic floor muscles are too weak to stop urine from leaking when you cough, laugh, or sneeze. Urge incontinence, or overactive bladder (OAB), occurs when urine leakage is closely preceded by a powerful urge to pass urine. It’s often a “I gotta go, gotta go, gotta go NOW," type of situation. Functional incontinence involves leakage when you struggle to get to the bathroom in time.
Read this post in its entirety:
Want to Improve Urinary Incontinence Symptoms? Try Physical Therapy
Tuesday, September 1, 2015
Accessing Your Medical Record
Did you know that you have a right to your medical records? It is the law. Most doctors and medical systems are now required to keep patient records in electronic format, called an electronic health record (EHR) or electronic medical record (EMR). But access to those records may not be easy and you may have to look in several places before you begin to find even a small portion of those records.
As a registered member of iConquerMS™ you are encouraged to submit EHRs to help fuel the largest patient-powered research network (PPRN) in the world to focus exclusively on multiple sclerosis.
What is an EHR?
Basically any electronic piece of information regarding your medical care can be considered an EHR. These digital records may include doctor’s notes, lab test results, MRI reports, x-rays, family medical history, prescription medications, history of surgeries, or even diagnostic and procedure codes used for insurance billing purposes.
How can I access my medical records?
- Visit summaries
Your doctor may provide you with a continuity of care document or summary at the end of each office visit which then becomes part of your medical record. To share this document with iConquerMS™, you can use your printer or a mobile app such as Genius Scan to scan it, save as a pdf, then upload it to the iConquerMS.org website.
- Paper records
You have the right to obtain a copy of your complete medical record, including doctor’s notes, but excluding notes related to mental health care. Doing so may become very expensive, however, with state-regulated charges for paper copies calculated per page. And, it is very likely that you would not know ahead of time how many pages would be included in your request. A modest 150-page record would cost $50 plus postage in Virginia.
- Patient portals
 Many healthcare systems are required to offer a patient portal through which information is made available. However, the amount of information which may be easily accessed varies considerably by system. You may find full MRI reports, laboratory test results, x-ray images, or continuity of care documents, but you most likely will not find detailed doctor’s notes.
Many healthcare systems are required to offer a patient portal through which information is made available. However, the amount of information which may be easily accessed varies considerably by system. You may find full MRI reports, laboratory test results, x-ray images, or continuity of care documents, but you most likely will not find detailed doctor’s notes.
If your healthcare system uses a “MyChart” patient portal powered by Epic Systems Corp, you may find the option to download your LUCY record which provides you with “a portable copy of your allergies, medications, current health issues, test results, and immunizations from MyChart.”
- Insurance claims
Some insurance companies offer portals through which you can view and download claims information and Explanation of Benefits (EOBs). 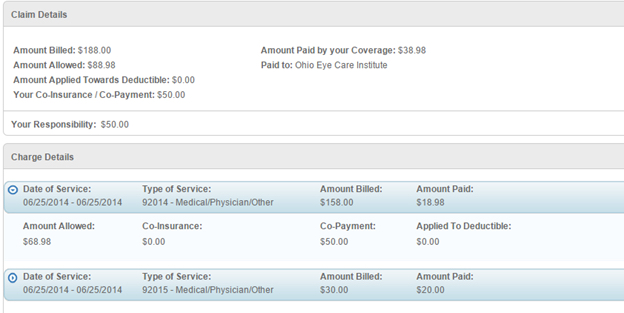 Although my company’s EOBs do not contain meaningful health information, some insurance companies may include diagnostic and procedural codes on their EOBs that provide value in a large database such as iConquerMS™.
Although my company’s EOBs do not contain meaningful health information, some insurance companies may include diagnostic and procedural codes on their EOBs that provide value in a large database such as iConquerMS™.
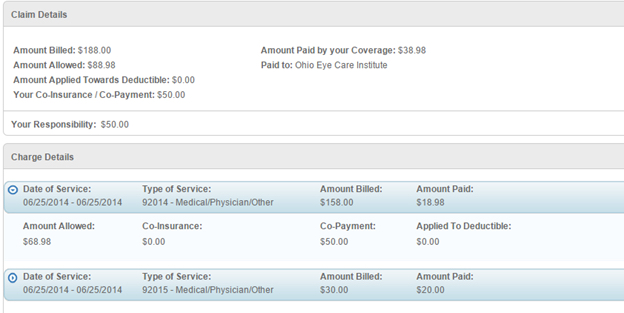 Although my company’s EOBs do not contain meaningful health information, some insurance companies may include diagnostic and procedural codes on their EOBs that provide value in a large database such as iConquerMS™.
Although my company’s EOBs do not contain meaningful health information, some insurance companies may include diagnostic and procedural codes on their EOBs that provide value in a large database such as iConquerMS™.
Why should I download my medical record?
As you will quickly see, no single doctor or healthcare system has your entire medical history and some of the information you find in your search may be contradictory, outdated, or inaccurate. As the patient, it is your right to collect and compile this information into a more complete record which you can check for errors and take with you to other doctors or facilities to same time and money.
If you are able to download portions of your medical record in pdf form through a patient portal, please do so. Not just for sharing with iConquerMS™, but also to begin building a folder of medical records you can keep on your computer.
Tuesday, August 25, 2015
Novartis Obtained MS Rights to Ofatumumab
What is ofatumumab?
Ofatumumab is a B-cell depleting monoclonal antibody therapy that targets CD20+ B-cells. Multiple sclerosis is known to be affected by T-cell activity, but is increasingly understood to be connected to B-cell activity in the immune system. B-cells are lymphocytes produced in the bone marrow.
B-cell depleting therapies and MS
Each of the investigational therapies that target CD20+ B-cells are cytotoxic, meaning that they bind to CD20 receptors on the cell surface and cause the cell to self-destruct. The rapid depletion of these specific B-cells is proving to be an effective treatment for MS.
Ofatumumab (Arzerra), a fully human MAB, has been studied in a small Phase IIa clinical trial involving 38 patients with relapsing-remitting MS. Results from the trial showed that intravenous ofatumumab (at each of three different doses being tested, given by infusions separated by two weeks) reduced total number of new brain lesions by up to 90% in 4-12 weeks. Compared to placebo, ofatumumab did not increase serious adverse events; however two patients in the 300-mg dosage group dropped out of the study because of adverse events. In light of these positive results, ofatumumab should be ready to move into Phase 3 trials.
Read this post in its entirety:
Novartis to Pay GSK $1B+ for Ofatumumab to Treat MS
Ofatumumab is a B-cell depleting monoclonal antibody therapy that targets CD20+ B-cells. Multiple sclerosis is known to be affected by T-cell activity, but is increasingly understood to be connected to B-cell activity in the immune system. B-cells are lymphocytes produced in the bone marrow.
B-cell depleting therapies and MS
Each of the investigational therapies that target CD20+ B-cells are cytotoxic, meaning that they bind to CD20 receptors on the cell surface and cause the cell to self-destruct. The rapid depletion of these specific B-cells is proving to be an effective treatment for MS.
Ofatumumab (Arzerra), a fully human MAB, has been studied in a small Phase IIa clinical trial involving 38 patients with relapsing-remitting MS. Results from the trial showed that intravenous ofatumumab (at each of three different doses being tested, given by infusions separated by two weeks) reduced total number of new brain lesions by up to 90% in 4-12 weeks. Compared to placebo, ofatumumab did not increase serious adverse events; however two patients in the 300-mg dosage group dropped out of the study because of adverse events. In light of these positive results, ofatumumab should be ready to move into Phase 3 trials.
Read this post in its entirety:
Novartis to Pay GSK $1B+ for Ofatumumab to Treat MS
Monday, August 24, 2015
Drug Assistance Programs You Should Know
Managing a chronic disease, such as rheumatoid arthritis, can be made more difficult if you are unable to afford your medications or health insurance premiums.
Copay assistance programs help patients who cannot afford to pay for prescribed medications despite insurance coverage. Frequently, drug manufacturers are able to provide financial help directly which should be your first resource to explore. To access manufacturer-sponsored programs, visit the brand website for the RA drug which you have been prescribed.
For patients who do not quality for manufacturer programs (perhaps due to insurance coverage through government programs such as Medicare), the following non-profit organizations offer additional help paying for medications. Some of these programs even offer financial help with insurance premiums and transportation costs to obtain treatment.
In general, to participate in these programs, the patient must have valid medical insurance that covers the prescribed medication, which in turn must be included on the program formulary; and the patient must meet annual household income criteria established by each program. One program included below offers help with generic medications regardless of insurance coverage.
Good Days from CDF
Read this post in its entirety:
Six Assistance Programs RA Patients Need to Know
Copay assistance programs help patients who cannot afford to pay for prescribed medications despite insurance coverage. Frequently, drug manufacturers are able to provide financial help directly which should be your first resource to explore. To access manufacturer-sponsored programs, visit the brand website for the RA drug which you have been prescribed.
For patients who do not quality for manufacturer programs (perhaps due to insurance coverage through government programs such as Medicare), the following non-profit organizations offer additional help paying for medications. Some of these programs even offer financial help with insurance premiums and transportation costs to obtain treatment.
In general, to participate in these programs, the patient must have valid medical insurance that covers the prescribed medication, which in turn must be included on the program formulary; and the patient must meet annual household income criteria established by each program. One program included below offers help with generic medications regardless of insurance coverage.
Good Days from CDF
- Good Days, formerly known as the Chronic Disease Fund, provides direct financial assistance to RA patients prescribed one of the following biologic drugs: Cimzia, Humira, or Remicade. To participate with Good Days, patients must remain fully compliant with their medication.
- Good Days offers a Premium Assistance Program that helps patients find, and pay for, appropriate health insurance coverage.
- The Good Days Travel Concierge Program offers transportation services for pre-approved medical appointments to obtain treatment. If needed, the program may also arrange and cover lodging. Additional travel expenses, such as parking, fuel and meals, are covered.
Read this post in its entirety:
Six Assistance Programs RA Patients Need to Know
Thursday, August 20, 2015
How to Take As Needed Medications
What does “as needed” mean?
Medications that are taken “as needed” are used only when necessary to treat a specific situation or symptom, such as pain, the common cold, allergies, constipation, anxiety, or fatigue. Some of these medications might be prescribed for you by a doctor while others can be purchased “over the counter” at your local pharmacy.
“Pro re nata” is a Latin phrase that means in the circumstances or as the circumstance arises. In medicine, pro re nata is abbreviated as p.r.n or PRN and means taken as needed or as the situation arises.
PRN medications are taken every once in a while to treat certain symptoms.
It is important to know what medications can be taken “as needed” and which ones must be taken regardless of how you feel. I take medications for low thyroid function, high cholesterol, and depression, each of which must be taken daily even if I feel great. This is non-negotiable. The list of medications I have on hand to be taken as needed is much longer and help me manage spasticity, nerve pain, anxiety, insomnia, and fatigue.
Can gabapentin or baclofen be taken “as needed”?
When I was first prescribed gabapentin and baclofen, I started them slowly, at a low dose, and titrated up to an effective dose which was taken daily on a regular schedule. Over the years, the amount of these medications I’ve needed to take has varied. At one point, I was taking 600mg of gabapentin three times daily to combat severe nerve pain. But now, I only take an occasional 300mg dose when mild nerve pain reaches the annoying or distracting stage. "As needed."
While I currently take baclofen each evening before bed, I also keep a prescription of diazepam (Valium) on hand for when the spasms get unbearable and when baclofen doesn’t sufficiently reduce the discomfort (ie, when massaging or stretching a knotted muscle causes intense crying).
Take medicines safely.
If you use PRN medications that are taken “only as needed,” it is important that you know exactly how these medications should be used. Discuss with your doctor his/her instructions regarding how frequently the medication can be used and what dosage you should use or not exceed.
Be aware that some of your PRN medications may be used instead of one of your other meds rather than in addition to. And, some medications may have similar ingredients and should not be used together. Ask your pharmacist if you ever have questions regarding medications (prescribed or OTC) to make sure that you take your medicines safely.
Read this post in its entirety:
Using "As Needed" Drugs with MS
(photo credit: Damian Gadal)
Thursday, August 13, 2015
10 Lessons I’ve Learned Since Being Diagnosed with MS
1. Be patient with yourself and others. Just like a baby isn’t born with the skills to run, jump, or do calculus, you are not suddenly equipped with all the knowledge and skills you need to handle every challenge caused by multiple sclerosis (MS). It takes time to grow and mature into living a good life with chronic illness, but doing so becomes easier more quickly if you don’t try to do it alone.
2. Don’t expect others to know what you need, what you are thinking, or what you are experiencing unless you share that information and are willing to talk about it openly and honestly. Communication is a vital component of life; use it to your advantage as you continue to improve your communication skills.
3. Doctors are ultimately our partners, not our gods or slaves. If you want to “be fixed” by medical professionals, it won’t happen. If you want to dictate every bit of your medical care, without allowing for an open dialogue (see #2), you will not receive the best care. Find a doctor with whom you can develop a good working relationship. Be honest with your doctor, and yourself, and trust that he/she is there to help you. If you cannot have this type of doctor-patient relationship, it is your responsibility to find a doctor with whom you can partner.
4. Be prepared to learn more than you ever wanted to know about health and the human body. While you are educating yourself, so that you can truly participate in your own care (see #3), stay curious about how the body works. Stay on top of the latest understandings about multiple sclerosis symptoms, causes, treatments, research, etc. Don’t become obsessed, but do become empowered with knowledge.
5. Seek the ‘silver lining’ in difficult circumstances. Maintaining a positive outlook is important for staying motivated to take care of yourself in all aspects of life. It can be too easy to live in despair, or to feel dwarfed by the barrage of challenges MS may throw at you. As long as you can hang onto a kernel of light, you can feed that light and watch it grow and shower your life with unexpected blessings.
6. MS may change your life, but it doesn’t change who you are down deep. Watching your hopes and dreams for the future effectively dissolve in front of your eyes is god-awful painful - don’t let anybody tell you otherwise - but you are much more than what you do (professionally). This is one lesson that I have to remind myself over and over again - each time I feel sad about having been on the verge of “making it” when MS intruded and changed the roadmap of my life. But most importantly, continue to have dreams.
7. Just as it’s okay to cry and get angry, it’s also okay to smile and feel happy. The most important thing (it seems to me) is to acknowledge your emotions, honor them, and to allow yourself to feel them fully. The more you allow positive emotions to flow, the greater they grow and thrive. The more you honor your own negative emotions, the more quickly they dissipate into smoke and float away.
8. A sign of strength is the willingness to ask for and accept help. You do not need to face challenges alone. As you practice to develop and improve your communication skills (see #2), it is important to allow others to contribute what they can to your overall well-being. Someday you will be rewarded with the opportunity to help someone else which you will see can be a blessing to both parties involved.
9. Life is less embarrassing than you think. Whether you are reluctant to have people visit because you haven’t cleaned your home to an artificial, perfect standard, or you pee your pants in a public bathroom and need to deal with wet clothing, moving beyond the embarrassment and getting on with enjoying life is vastly more important than closing yourself off from others physically or emotionally.
10. Focus on what you CAN do today to make life better for yourself. No matter what your challenges, there are endless possibilities and actions you can take to improve your circumstances. Somedays, I have to move away from struggling to stay alert to “get work done” - a CAN’T situation - to focusing on listening to my body and giving it what it may need today which is a 2 o’clock nap and cuddle with a soft, fuzzy kitty cat - definitely a CAN DO situation.
What lessons have you learned since being diagnosed with MS or any other chronic disease? Share in the comments and you may end up completing #8!
This post originally appeared on HealthCentral.
(photo credit: deathtothestockphoto.com)
Subscribe to:
Posts (Atom)



